An Unlikely Connection Between Familial Mediterranean Fever (FMF) and the Bubonic Plague
Genetics and Pathology of Familial Mediterranean Fever (FMF)
Familial Mediterranean Fever (FMF), also known as familial paroxysmal polyserositis or recurrent polyserositis, is an autoinflammatory syndrome that is identified by recurring inflammation of the trunk and joints.1-3 These episodes of inflammation can last from 12 hours to 3 days and are associated with high fever, abdominal pain, painful skin lesions, and transient arthritis.1-3 Time between episodes ranges from several days to several years, depending on the severity of the disease.2 Average onset of FMF occurs in childhood.2
It is important to note that FMF is an autoinflammatory syndrome and not an autoimmune syndrome, like amyotrophic lateral sclerosis (ALS). In autoimmune disorders, the adaptive immune system malfunctions and mistakenly attacks healthy tissue. For example, in ALS, the immune system wrongly attacks and degrades nerve cells in the spinal cord and brain, leading to gradual paralysis. In contrast, autoinflammatory disorders like FMF involve an abnormality of the innate immune system that causes periodic episodes of inflammation in the immune system. The innate immune system is composed of general immune safeguards such as physical barriers and protective molecules, whereas the adaptive immune system develops specific responses.
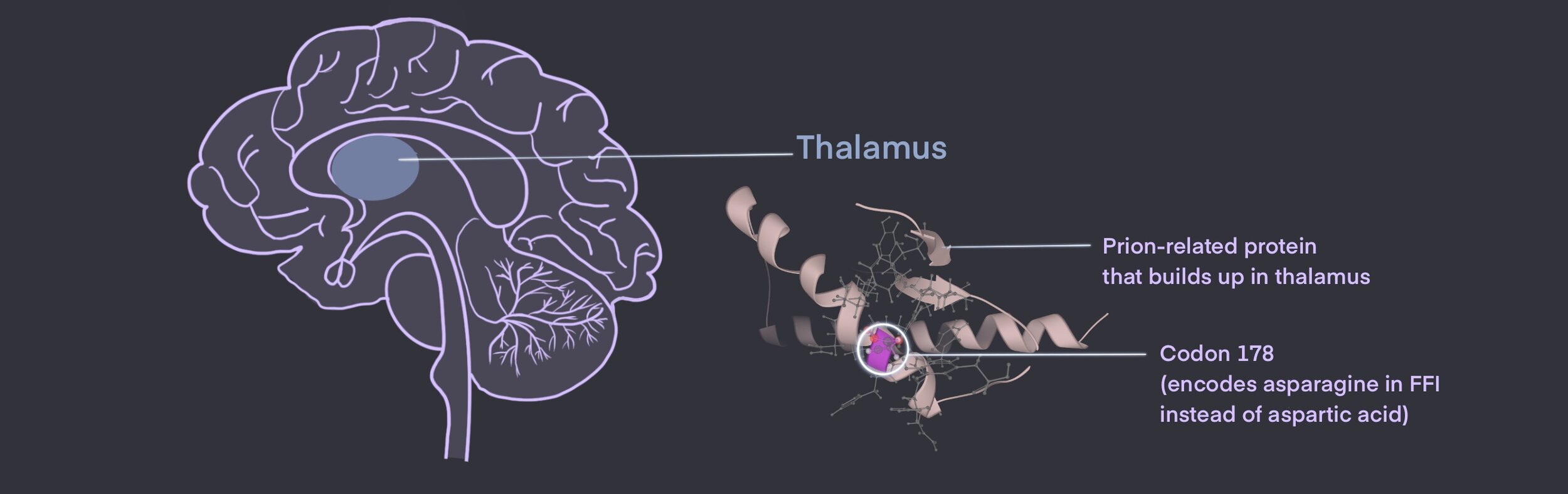
FMF is typically an autosomal recessive disorder, although some instances of autosomal dominance have also been reported.1,3,4 In autosomal recessive genetic disorders, one copy of the mutated gene is inherited from each parent and both copies are required to cause symptoms. FMF is caused by a mutation in the Mediterranean fever (MEFV) gene found on chromosome 16.1,4 Although ~310 MEFV sequence variances have been documented, to date only 4 specific mutations are associated with developing FMF.1,4 These pathogenic mutations cause pyrin, the protein normally encoded by MEFV, to be hyperactive. Normally, pyrin exists in immune cells such as neutrophils and macrophages. Once activated by the innate immune system, pyrin triggers the release of proinflammatory proteins (known as cytokines) such as interleukin-1ꞵ (IL-1ꞵ) and interleukin-18 (IL-18), which are small molecules that amplify bodily mechanisms to combat pathogens. However, abnormal pyrin found in FMF causes an exaggerated immune response by overproducing cytokines, even in the absence of pathogens, thus causing inflammation of organ membranes and giving rise to FMF symptoms.4,5
Past Research
Interestingly, FMF incidence is the highest in people of East Mediterranean ethnicity, including those of North African, Jewish, Arab, Armenian, Turkish, Greek, and Italian descent (hence the Mediterranean in FMF).1-3,5 It is reported that ~8% of people in the East Mediterranean basin carry one of the disease-causing MEFV mutations.5 With the advance of genetic and molecular experimental techniques, researchers at the National Human Genome Research Institute (NHGRI) recently proposed that the commonality of this mutation within East Mediterranean ethnicities may provide some protection against infection by Yersinia pestis in the bubonic plague.5,6 This is a pivotal hypothesis that may offer an explanation for the evolutionary selection of FMF within those of East Mediterranean ethnicity.
It is thus important to understand the history, etiology, and infection mechanism of the bubonic plague. The first wave of the bubonic plague occurred in 541 CE and two subsequent waves occurred in the following two thousand years, cumulatively killing over 50 million people.7 Cases occurred around the world, including in the Mediterranean basin, across Europe, and in China. The bubonic plague is caused by Y. pestis, a bacterial agent transmitted by fleas (Xenopsylla cheopis), which are transported by the black rat (Rattus).7
The logic behind FMF conferring protection against the bubonic plague stems from how the bacterial agent affects the host’s immune system. Infection by Y. pestis causes the release of a molecule known as YopM, which binds to pyrin and reduces the production of inflammatory cytokines. This reduction in cytokines will suppress the innate immune system and allow the virus to multiply itself and ravage the body.7-9 However, since those who carry the MEFV mutation are constantly producing inflammatory cytokines, it is thought that Y. pestis will not be able to suppress the immune system and may die out faster, thus producing less severe symptoms of bubonic plague. So it may be plausible that evolutionary selection favored individuals with the MEFV mutation since they were less likely to die from the plague. Although it may seem odd that genetic disease may be evolutionarily favored, it is a matter of which scenario improves the chance for reproduction. Diseases that offer a greater chance to reproduce before causing the host to die are evolutionarily more favored than diseases which cause death before reproduction.
Current Research
In the landmark study by Park et al., they tested the hypothesis that having FMF can be protective against the plague via a variety of experiments.7-9 Firstly, genetic analysis of about 2000 Turkish people and 300 archaeological samples revealed that FMF mutations are relatively common in the Turkish population and plausibly occurred 1800-2600 years ago (around the same time as the first wave of the plague). Secondly, by exposing isolated immune cells from FMF patients and non-FMF patients to Y. pestis in vitro they found that the binding of YopM to pyrin was reduced and IL-1ꞵ release was higher in FMF cells compared to the controls. This supports the notion that FMF mutations are protective against the efforts of Y. pestis to suppress the innate immune system. Thirdly, the Park et al. in vivo experiment in FMF mice model infected with Y. pestis showed that mice with FMF mutations had higher survival than controls. Overall, the authors concluded that the bubonic plague probably had a role in selecting for FMF-causing mutations in the East Mediterranean population.9
This study demonstrates that epidemics can have long-lasting impacts on humans’ physiology and genetics, potentially engaging in positive selection of new genetic diseases. As such, studying FMF in the context of the COVID-19 pandemic can be instructive since both SARS-CoV2 and FMF affect the immune system (formerby overactivating, latter by suppressing it). Even if this line of questioning doesn’t yield conclusive treatment, the greater lesson to be learned is that the study of rare diseases provides valuable research to the entire medical discipline and cannot be discounted.
Vaishnavi BhamidiReferences:
1. Familial Mediterranean Fever. NORD (National Organization for Rare Disorders). Accessed February 13, 2021. https://rarediseases.org/rare-diseases/familial-mediterranean-fever/
2. Familial Mediterranean fever - Symptoms and Causes. Mayo Clinic. Accessed February 13, 2021. https://www.mayoclinic.org/diseases-conditions/familial-mediterranean-fever/symptoms-causes/syc-20372470
3. Bashardoust B. Familial Mediterranean fever; diagnosis, treatment, and complications. J Nephropharmacol. 2015;4(1):5-8.
4. Seza Özen, Ezgi Deniz Batu, Selcan Demir. Familial Mediterranean Fever: Recent Developments in Pathogenesis and New Recommendations for Management. Front Immunol. 2017;8. doi:10.3389/fimmu.2017.00253
5. Patin E. Plague as a cause for Familial Mediterranean Fever. Nat Immunol. 2020;21(8):823-824. doi:10.1038/s41590-020-0735-0
6. Prabarna Ganguly. Ancient disease could protect some from the bubonic plague. National Human Genome Institute. Published June 29, 2020. Accessed February 22, 2021. https://www.genome.gov/news/news-release/genomic-variation-causing-common-autoinflammatory-disease-may-increase-resilience-to-bubonic-plague
7. Glatter KA, Finkelman P. History of the Plague: An Ancient Pandemic for the Age of COVID-19. The American Journal of Medicine. 2021;134(2):176-181. doi:10.1016/j.amjmed.2020.08.019
8. Ratner D, Orning MPA, Proulx MK, et al. The Yersinia pestis Effector YopM Inhibits Pyrin Inflammasome Activation. Brodsky IE, ed. PLoS Pathog. 2016;12(12):e1006035. doi:10.1371/journal.ppat.1006035
9. Park YH, Remmers EF, Lee W, et al. Ancient familial Mediterranean fever mutations in human pyrin and resistance to Yersinia pestis. Nature Immunology. 2020;21(8):857-867. doi:10.1038/s41590-020-0705-6
Cite This Article:
Bhamidi, V., Chen, L., Charron, B., Vinokurtseva, A., Chharawala, V., Ananthakrishnan, O., Lombo, L. An Unlikely Connection Between Familial Mediterranean Fever and the Bubonic Plague. Illustrated by Chen K. Rare Disease Review. June 2024. DOI: 10.13140/RG.2.2.33735.20643